Dysphagia (Difficulty Swallowing)
Difficulty in swallowing (dysphagia) is common among all age groups, especially the elderly. The term dysphagia refers to the feeling of difficulty passing food or liquid from the mouth to the stomach. This may be caused by many factors, most of which are temporary and not threatening. Difficulties in swallowing rarely represent a more serious disease, such as a tumor or a progressive neurological disorder.
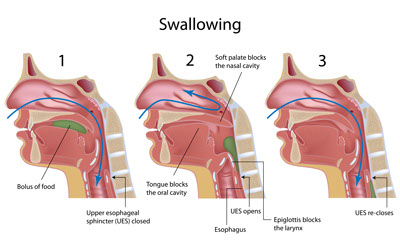
People normally swallow hundreds of times a day to eat solids, drink liquids, and swallow the normal saliva and mucus that the body produces. The process of swallowing has four related stages:
- The first stage is the oral preparation stage, where food or liquid is manipulated and chewed in preparation for swallowing.
- The second stage is the oral stage, where the tongue propels the food or liquid to the back of the mouth, starting the swallowing response.
- The third stage is the pharyngeal stage, which begins as food or liquid is quickly passed through the pharynx (the region of the throat which connects the mouth with the esophagus), and then into the esophagus.
- In the final, esophageal stage, the food or liquid passes through the esophagus into the stomach.
Although the first and second stages have some voluntary control, stages three and four occur involuntarily, without conscious input.

Any interruption in the swallowing process can cause difficulties. One of the most common causes of dysphagia is laryngopharyngeal reflux. In this condition stomach acid moves up the esophagus to the pharynx, causing inflammation and irritation of the tissues in the throat. Other causes may include: hypertension, diabetes, thyroid disease, stroke, progressive neurologic disorder, the presence of a tracheotomy tube, a paralyzed or weak vocal cord, a tumor in the mouth, throat, or esophagus, or surgery in the head, neck, or esophageal areas.
Swallowing difficulty can also be connected to some medications including Nitrates, Anticholinergic agents (found in certain anti-depressants and allergy medications), Calcium tablets, Calcium channel blockers, Aspirin, Iron tablets, Vitamin C, Antipsychotics and Tetracycline (antibiotic used to treat certain infections and acne).
Symptoms of swallowing disorders may include drooling, a feeling of food or liquid getting stuck in the throat, discomfort in the throat or chest, a “foreign body” or “lump-like” sensation in the throat, coughing or choking when swallowing, or change in voice.
Evaluation
The specialists at New England ENT offer diagnostic evaluations and various treatment options for your swallowing problems. Evaluation includes a thorough history of a patient’s hoarseness and general health, as well a complete ear, nose, and throat exam. Examination may include the use of a very small, lighted flexible tube (fiberoptic scope) that is passed through the nose to view the throat and voice box. We also offer FEESST (Flexible Endoscopic Evaluation of Swallowing with Sensory Testing) where the swallowing process is evaluated and recorded using the fiberoptic scope. We work closely with Speech & Language Pathologists who can also evaluate a patient’s swallowing to help diagnose the underlying problem and guide appropriate treatment.
New England ENT is one of the few centers in the country to offer a highly sensitive, outpatient diagnostic test (Restech Dx-pH Measurement system) to quantitatively measure the degree of reflux into the throat. This is a simple, comfortable test performed with a small probe containing a senor at the tip. It is passed through the nose until the tip is at the back of the throat (high enough that patients cannot feel it when speaking or swallowing). The probe wirelessly records the acid exposure (every 30 seconds) over a 24-hour period. Patients can eat normal meals, go to work and even exercise during the testing period. With the patient’s input, the Dx-System tracks meals, symptoms and supine periods. This helps correlate symptoms and reflux patterns. This is a valuable tool in the comprehensive assessment of patients with laryngopharyngeal reflux.

Treatment
Many swallowing disorders can be treated with medication and swallowing therapy. Treatment is tailored to the particular cause of the swallowing disorder. Once the cause is determined, swallowing disorders may be treated with:
- Medications
- Swallowing therapy
- Surgery
Laryngopharyngeal reflux can often be treated with medications to control stomach acid production, and by changing eating and living habits in these ways:
- Eat a bland diet with smaller, more frequent meals.
- Eliminate tobacco, alcohol and caffeine.
- Reduce weight and stress.
- Avoid food within three hours of bedtime.
- Elevate the head of the bed at night.
Many swallowing disorders may be helped by direct swallowing therapy. A Speech & Language Pathologist can provide special exercises for coordinating the swallowing muscles or stimulating the nerves that trigger the swallow reflex. Patients may also be taught simple ways to place food in the mouth or position the body and head to help the swallow occur successfully. Some patients with swallowing disorders have difficulty in feeding themselves. An occupational therapist or Speech & Language Pathologist can aid the patient and family in feeding techniques. These techniques make the patient as independent as possible. A dietician or nutritional expert can determine the amount of food or liquid necessary to sustain an individual and whether supplements are necessary.
Surgery is used to treat certain problems. If a narrowing exists in the throat or esophagus, the area may need to be stretched or dilated. If a muscle is too tight, it may need to be dilated or released surgically. This procedure is called a cricopharyngeal myotomy and can be performed trans-orally without the need for external incisions and prolonged hospital stay.
