Squamous Cell Cancer
Squamous cell carcinomas are the most common type of head and neck cancer and arise from epithelial cells that line the mucosal surfaces in the head and neck.
Oral cavity (lips, front two-thirds of the tongue, gums, lining inside the cheeks and lips, floor of the mouth under the tongue, hard palate, and the area of the gums behind the wisdom teeth)
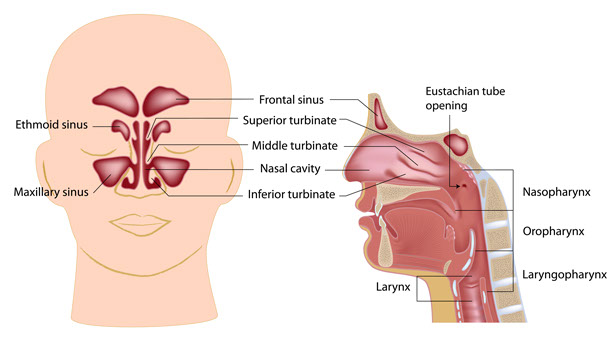
Pharynx (an area extending from behind the nose and leading to the esophagus). It is further divided into three parts:
- Nasopharynx (upper part of the pharynx, behind the nose)
- Oropharynx (middle part of the pharynx, including the soft palate, base of tongue, and tonsils)
- Hypopharynx (lower part of the pharynx around the larynx and leading to the esophagus)
Larynx (voice box). It is further divided into three parts:
- Supraglottis (epiglottis, and tissues above the vocal cords)
- Glottis (vocal cords)
- Subglottis (tissues below the vocal cords)
Nasal cavity and paranasal sinuses (air-filled space within the nose and hollow spaces in the bones of the head surrounding the nose)
- Salivary glands (paired glands near the jawbone and in the floor of the mouth which secrete saliva)
- Thyroid (bilobed ductless gland in the neck in front of the trachea which secretes hormones regulating metabolism)
In some instances, cancer cells can be found in the lymph nodes of the neck without evidence of cancer in any of the aforementioned areas. This is called metastatic squamous cell carcinoma with unknown (occult) primary.
Risk Factors

The most important risk factors for head and neck cancers are alcohol and tobacco use (including use of smokeless tobacco). Over 75% of head and neck cancers are associated with alcohol and tobacco use. The concomitant use of tobacco and alcohol confers a 100-fold increased risk of developing these cancers than the use of either product alone. Tobacco and alcohol are not risk factors for salivary gland or thyroid cancers.
Over the past thirty years, Infection with human papillomavirus (HPV) has become a significant risk factor for certain types of head and neck cancers, particularly in the oropharynx.
Other specific risk factors for developing cancer in various regions of the head and neck are described below:
- Oral cavity: sun exposure (lip); poor oral hygiene and missing teeth; use of harsh oral care products; chewing paan (betel quid); consumption of mate (a tea-like beverage).
- Nasopharynx: Chinese ancestry; Epstein-Barr Virus (EBV) infection; occupational exposure to wood dust; consumption of certain preservatives or salted foods.
- Hypopharynx: Plummer-Vinson (also called Paterson-Kelly) syndrome–a rare disorder that results from iron and other nutritional deficiencies causing severe anemia and esophageal webs.
- Larynx: certain industrial exposures, including asbestos and synthetic fibers; occupational exposures in the construction, metal, textile, ceramic, logging, and food industries; consumption of mate.
- Nasal cavity and paranasal sinuses: certain industrial exposures such as wood, nickel dust or formaldehyde.
- Thyroid: exposure to radiation (particularly as a child) from medical treatments or radiation fallout from power plants and nuclear weapons; gender (females carry a 3-fold risk when compared to men); diet low in iodine (risk for follicular thyroid cancers in certain parts of the world); hereditary factors.
Symptoms
The signs and symptoms of head and neck cancers commonly include a lump or sore that does not heal or go away, painful or difficulty swallowing, ear pain without an ear infection and a change in voice. Specific signs and symptoms may also include:
- Oral cavity: white or red patch in the mouth; swelling of the jaw that causes dentures to fit poorly or become uncomfortable; unusual pain or bleeding.
- Pharynx: difficulty breathing or speaking; decreased hearing (nasopharynx).
- Larynx: voice changes, coughing up blood, painful or difficulty swallowing
- Nasal cavity and paranasal sinuses: chronic sinus infections that do not respond to treatment; nosebleeds; headaches; vision changes; pain in the upper teeth; problems with dentures.
- Salivary gland: swelling around the jawbone or under the chin; infection of the salivary gland that does not respond to treatment; paralysis of the muscles of the face.
- Thyroid: typically asymptomatic, especially early in its development; larger or more aggressive cancers may present with symptoms of pain in the neck, difficulty swallowing or breathing, and hoarseness.
Evaluation
Patients suspected of having a head and neck cancer should seek an Otolaryngologist – Head & Neck Surgeon for a consultation. A thorough medical history and physical examination is performed, focusing on the head and neck. Specialized diagnostic procedures can be performed in the office to help identify and diagnose a cancer. The ability to fully evaluate areas such as the larynx and pharynx has advanced greatly with the use of a flexible fiberoptic laryngoscope, where a thin fiberoptic camera with an internal light source is passed through the nose to visualize the upper aero-digestive tract from the nasal cavities to the larynx (voicebox).
Other diagnostic procedures which are often performed include ultrasound, CAT scan, MRI, PET scan, videostroboscopy and fine needle aspiration, or tissue biopsy. PET-CT (Positron Emissions Tomography – Computed Tomography) combines the areas of high glucose metabolism seen in cancer cells and overlays this information over the anatomic images from a CT scan. This allows for identifying specific areas of the primary cancer, regional lymph node spread and distant metastasis. For patients with a cancer in the upper aero-digestive tract, a complete evaluation may require panendoscopy. This involves the surgeon fully assessing the extent of the primary cancer and evaluating for any secondary cancers while the patient is under general anesthesia using specialized instruments.
Surgery
Surgery has been an integral treatment modality for head and neck cancer patient over the past century. Surgical goals balance complete extirpation of the primary and any regional metastatic disease with maintenance of form and function. With advancements in technology and surgical reconstructive techniques, patients with advanced cancers can still be offered a surgical treatment with minimal morbidity and favorable functional outcomes as detailed below:

- Laser-assisted Surgical Therapy – Laser therapy has been an integral tool to the treatment of soft tissue head and neck cancers for over 40 years. Combining precision and accessibility is a direct advantage of using laser therapy during endoscopic procedures for the larynx and base of tongue.
- Nerve Monitoring – Preservation of certain nerves not involved with cancer is a high priority to improve post-operative functional abilities for head and neck cancer patients. Intra-operative nerve monitoring is routinely used in thyroid and parotid gland surgery to minimize the risk of injury to the recurrent laryngeal nerve (in thyroid surgery) to prevent vocal cord dysfunction and hoarseness, and the facial nerve (in parotid gland surgery) to help prevent facial paralysis post-operatively.
- Harmonic Scalpel – The head and neck region is one of the most complex anatomic areas of the human body with a robust blood supply to each region. The Harmonic scalpel is used during surgery to efficiently dissect through tissue and divide small-to medium-sized blood vessels, with minimal risk of post-operative bleeding and reduced total operative time.
- Transoral Robotic Surgery (TORS) – With its inception primarily in Urologic and Gynecological Oncologic surgery, Robotic Surgery is now being used to help treat patients with early stage oropharyngeal cancers involving the pharynx, tonsil or base of tongue. TORS is a minimally invasive approach for patients who would have otherwise required an extensive open procedure or would have been unresectable.
- Free Flap Reconstruction – One of the most exciting aspects of head and neck reconstructive surgery is the introduction of free tissue transfer to help improve the function and cosmesis. Large defects secondary to extensive surgical cancer resection can be reconstructed using skin, muscle and sometimes from other sites of the body, such as the forearm, lower leg, abdomen and scapula.
Survival

One of the most critical means of improving prognosis and survival from a head and neck cancer is with early detection. Overall survival worsens as the stage of the disease advances. Despite improvements in diagnosis and local management, long-term survival rates in head and neck cancer have not increased significantly over the past 40 years, and are among the lowest worldwide of the major cancers. The problem is even worse for select populations such as African Americans, for whom survival rates have actually decreased. Oropharyngeal cancer, the largest subgroup of head and neck cancers, has a 5-year relative survival rate of only 59% for whites and 35% for blacks in the United States.
Although early-stage head and neck cancers (especially laryngeal and oral cavity) have high cure rates, over 60% of head and neck cancer patients present with advanced disease. Cure rates decrease in locally advanced cases, whose probability of cure is inversely related to tumor size and even more so to the extent of regional node involvement. Of particular interest, recent investigations have identified a subset of patients with HPV-related cancers presenting with smaller primary tumors and bulky regional metastatic nodes, but with improved overall survival rates.
Head & Neck cancer five-year disease-specific survival can range from over 90% in stage I patients to less than 50% in Stage IV patients. Long-term survival outcomes specifically for thyroid cancers are quite favorable compared to other head and neck cancers. The long-term 20-year survival for patients with thyroid cancer approaches 90%.
