Thyroid Surgery
Introduction
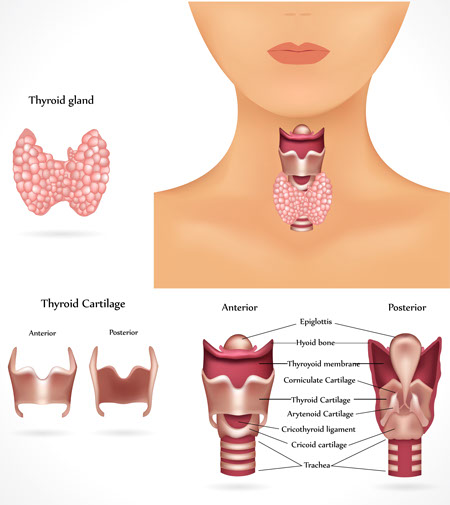
The thyroid gland is part of the endocrine system that makes hormones to regulate physiological functions in your body, like metabolism (heart rate, sweating, energy consumed). Other endocrine glands include the pituitary, adrenal, parathyroid glands and specialized cells within the pancreas. The thyroid gland is located in the middle of the lower neck, below the larynx (voice box) and wraps around the front half of the trachea (windpipe). It is shaped like a bow tie, just above the collarbones, having two halves (lobes) joined by a small bridge of tissue (isthmus.).
Diseases of the thyroid gland are very common, affecting millions of Americans. The most common thyroid problems are:
- An overactive gland, called hyperthyroidism (e.g., Graves’ disease, toxic adenoma or toxic nodular goiter
- An underactive gland, called hypothyroidism (e.g., Hashimoto’s thyroiditis)
- Thyroid enlargement due to over-activity (as in Graves’ disease) or from under-activity (as in hypothyroidism). An enlarged thyroid gland is often called a “goiter.”
- Thyroid masses (nodules), which could be benign or cancerous (malignant). Most thyroid nodules are benign. Patients with a family history of thyroid cancer or who had radiation therapy to the head or neck as children for acne, adenoids, or other reasons are more prone to develop thyroid cancer.
Diagnosis
The diagnosis of a thyroid function abnormality or thyroid mass is made by taking a detailed medical history and a physical examination. As part of the exam, your doctor may also examine the voice box (larynx) with a fiber-optic scope to evaluate vocal cord function. Tests your doctor may order include:
- Ultrasound examination of the neck and thyroid
- CT or MRI of the neck and chest
- Blood tests of thyroid function
- Fine-needle aspiration (FNA) biopsy
Thyroid Cancer
Thyroid cancer is commonly diagnosed at a younger age than most other adult cancers. Nearly 2 out of 3 cases are found in people younger than 55 years of age. There is a gender predilection, with thyroid cancers presenting 3 times more commonly in women than in men. The chance of being diagnosed with thyroid cancer has risen in recent years, and is now more than twice as likely as it was in 1990. This is partly a result of the increased use of imaging studies of the head & neck and chest, which could incidentally detect small thyroid nodules that might not have otherwise been found in the past. However, the death rate from thyroid cancer has been fairly stable for many years, and remains very low compared with most other cancers.
The thyroid gland contains two types of cells: follicular cells, which are responsible for the production of thyroid hormone, and C cells, which make Calcitonin, a hormone that participates in calcium metabolism. There are four main types of thyroid cancer:
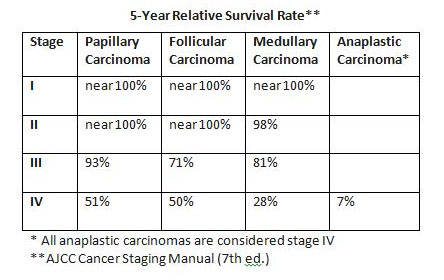
Papillary thyroid cancer: Papillary thyroid cancer develops from the follicular cells and grows slowly. It is the most common type, comprising 85% of all thyroid cancers. It is usually found in one lobe, and only 10-20% of papillary thyroid cancers appear in both lobes. Papillary thyroid cancer is a well-differentiated thyroid cancer, meaning that the tumor looks similar to normal thyroid tissue under a microscope.
Follicular thyroid cancer: Follicular thyroid cancer is the second most common type of thyroid cancer, and affects 10% of patients presenting with thyroid cancer. It also develops from the follicular cells and usually grows slowly. Follicular thyroid cancer is also a well-differentiated thyroid cancer. Papillary and Follicular thyroid cancers are very often curable, especially when found early and in patients younger than 45 years of age.
Medullary thyroid cancer (MTC): MTC develops in the C cells and is sometimes the result of a genetic syndrome called multiple endocrine neoplasia type 2 (MEN2). This tumor has very little, if any, similarity to normal thyroid tissue. MTC can often be controlled if it is diagnosed and treated before it spreads to other parts of the body. MTC accounts for about 3% of thyroid cancers. Medullary thyroid cancer sometimes runs in families. A change in a gene called RET can be passed from parent to child. Nearly everyone with a changed RET gene develops medullary thyroid cancer. The disease occurs alone, as familial medullary thyroid cancer, or with other cancers, as multiple endocrine neoplasia (MEN) syndrome. A blood test can usually detect a changed RET gene. If it is found in a person with medullary thyroid cancer, the doctor may suggest that family members also be tested. For those who have a changed gene, frequent lab tests or surgery may be recommended to remove the thyroid before cancer develops.
Anaplastic thyroid cancer: This type is rare, accounting for about 1% of thyroid cancers. It is a fast-growing, poorly differentiated thyroid cancer that starts from differentiated thyroid cancer or a benign tumor of the gland. Anaplastic thyroid cancer can be sub-typed into giant cell classifications. Because this type of cancer grows so quickly, it is more difficult to treat successfully.
Thyroid Surgery
The board-certified specialists at New England ENT are some of the most experienced thyroid surgeons in the Merrimack Valley, and routinely perform surgeries for:
- A thyroid mass (nodule), which has been biopsied and reported as indeterminate, suspicious or suggestive of cancer.
- Enlarged thyroid gland (goiter) causing symptoms such as difficulty swallowing or shortness of breath. Surgery is also considered for large goiters without symptoms, if there is evidence of progressive growth or extension below the neck into the chest cavity.
- Overactive gland (hyperthyroidism) when medications are ineffective or not tolerated by the patient.
Thyroid surgery is an operation performed to remove part or all of the thyroid gland. It is performed in the hospital, and general anesthesia is usually required. Typically, the operation removes the lobe of the thyroid gland containing the lump and possibly the isthmus. A frozen section (immediate microscopic reading) may be used to determine if the rest of the thyroid gland should be removed during the same surgery. Sometimes, based on the result of the frozen section, the surgeon may decide not to remove any additional thyroid tissue, or proceed to remove the entire thyroid gland, and/or other tissue in the neck. This decision is usually made in the operating room by the surgeon, based on findings at the time of surgery. Your surgeon will discuss these options with you preoperatively. As an alternative, your surgeon may choose to remove only one lobe and await the final pathology report before deciding if the remaining lobe needs to be removed. There also may be times when the definite microscopic answer cannot be determined until several days after surgery. If a malignancy is identified in this manner, your surgeon may recommend that the remaining lobe of the thyroid be removed at a second procedure.
Patients may also be referred to other specialists, such as endocrinologists, nuclear medicine specialists, medical and radiation oncologists for further treatment and continued surveillance after surgery.


Examples of post-operative scar 6 mos-1 yr after Thyroid Surgery
